Homeopathy & Irritable Bowel Syndrome (v. II)
Stress restricts recovery and increases harmful commensal intestinal bacteria
Homeopathy, with its potential to address mental, emotional and physical symptoms concurrently, is an increasingly popular treatment option for people suffering irritable bowel syndrome, a complex multi-symptomatic disorder requiring interdisciplinary, gastroenterological and psychotherapeutic, treatments. Observational studies of homeopathy in chronic disease are promising but its role in irritable bowel syndrome is less clear, with two systematic reviews unable to confirm or deny its efficacy.
Irritable bowel syndrome (IBS) is a chronic disease which significantly reduces quality of life (QOL)(1) and usual medical diagnosis for unexplained gastrointestinal symptoms. With global prevalence estimated at 4.1%(2) IBS incurs significant health care costs(3) and is the most common functional gastrointestinal disorder.
Although a personalized approach using pharmacological, dietary and psychologic interventions is recommended,(4) reduced QOL, significant disability, and impaired workforce productivity(5) leaves many IBS patients dissatisfied with their medical care(6) necessitating continued clinical efficacy, safety and cost-effectiveness studies for approved and non-approved IBS treatments.(7)
Pathophysiology of IBS
IBS typically presents with abdominal pain and accompanying stool changes. There are four subtypes diagnosed by Rome IV criteria:(8)
IBS-C constipation predominant.
IBS-D diarrhoea predominant.
IBS-M alternating diarrhoea and constipation.
IBS-U unspecified, having variable symptoms.
The pathology of IBS is not well understood but includes altered gastrointestinal motility, (9) increased intestinal permeability,(10) visceral hypersensitivity, and low-grade inflammation.(11)
Pathogenesis of gastrointestinal infection has been identified(12) in 5% to 32% of cases,(13) associated with small intestinal bacterial overgrowth (SIBO) in up to 78% of diagnoses,(14) and fungal dysbiosis.(15) Dysbiotic commensal bacterial communities are implicated(16) with somatization,(17,18) and differ between subtypes.(19)
Altered faecal and mucosal-associated microbial composition are connected to(19-24) and essential in understanding individual IBS symptom pictures.(25) Many medical treatments irrevocably denude the microbiome triggering chronic immune dysfunction and inflammation.(19-23,26)
IBS is a gut-brain interaction disorder(27,28) with 50% of sufferers experiencing gastrointestinal symptoms only.(29) Co-occurrence with anxiety / depression is 44 to 84%,(30) with somatic comorbidities including agoraphobia, and insomnia(11) associated with more severe symptoms, reduced QOL, and increased physical and mental distress.(17) Panic, neurasthenic and depressive disorders consistently result in poorer IBS outcomes,(31) and require psychotherapeutic treatment.(32) Serotonin (5-hydroxytryptamine), a major pathophysiogenic factor in IBS, has a prominent role in controlling gastrointestinal motility.(33)
Psychosocial IBS research, via the maternal separation animal model, has shown this early life stressor induces colonic hyper-contraction, gastric hypersensitivity, and delayed emptying.(16) The stress response restricts recovery(34) and increases harmful commensal intestinal bacteria(35) in IBS which is also classified as a functional somatic syndrome.(11,17)
Australian prevalence of IBS is 14% using Rome I, II, III;(36) 8.9% by Rome II;(37) and 3.5% via Rome IV – rates of Rome IV diagnosed IBS are much lower than in earlier incarnations of the Rome criteria.(2,38)
Current IBS treatments
Low quality pharmacologic and non-pharmacologic IBS studies make treatment guidelines challenging.(39) The American College of Gastroenterology recommends chloride channel activators and guanylate cyclase activators for global IBS-C, and rifaximin in global IBS-D(1) although it has lower efficacy than alosetron and eluxadoline.(7) Antispasmodics provide short term symptom relief comprising first-line treatment for pain-predominant IBS and IBS-D(7) but induce adverse, anticholinergic effects.(40) Linaclotide improves stool frequency, constipation severity, and abdominal pain and discomfort in IBS-C,(40) but tenapanor is expected to take its place.(7) Over the counter laxatives may relieve IBS-C constipation without treating abdominal pain and discomfort.(40)
Gut-brain neuromodulators are prescribed for moderate to severe IBS associated with pain or comorbid psychological disorders.(7) Tricyclic antidepressants, selective serotonin reuptake inhibitors, and serotonin-norepinephrine reuptake inhibitors are known to induce global symptom relief and improve abdominal discomfort.(39,40) Addressing psychological wellbeing improves IBS outcomes(42) with psychological interventions improving overall symptoms and relieving abdominal pain.(39) Gut-directed psychotherapy and a low fermentable oligosaccharide, disaccharide, monosaccharide and polyol (FODMAP) diet are routinely recommended for global IBS symptoms.(1) Evidence for the use of probiotics is mounting but specific strains and molecular targets remain to be determined.(27) Cognitive Behavioural Therapy interventions and gut-directed hypnotherapy have proven efficacious in long-term treatment,(42) with an Australian trial showing gut-directed hypnotherapy as effective as a low-FODMAP diet.(43)
Hausteiner-Wiehle and Henningsen(29) implored treatment structures abandon classification of purely organic or purely mental disorders by acknowledging the variability of IBS through awareness of extraintestinal and psychobehavioural symptoms, and the implementation of a collaborative care model as IBS is a multifactorial disease requiring clinical, psychological, and biochemical evaluation.(17)
Complementary Medicine may be beneficial for global IBS symptoms,(44) with mucoprotectants providing some protection against altered intestinal permeability, dysbiosis, and mucosal micro-inflammation in IBS-D.(45) Gut-brain axis interaction induced by Chinese medicines have been noted in several studies,(46) and acupuncture has shown IBS treatment effects lasting up to 12 weeks.(47) Systematic review showed a little overall IBS symptom improvement after homeopathic treatment but, as for all IBS treatment studies, certainty of evidence is low.(39,44)
Homeopathy
Gastroenterological complaints are commonly seen in professional homeopathic practice.(48) Homeopathy, a therapeutic medical system based on the theory of like cures like - that disease can be addressed via the use of the substance which produces similar symptoms to the disease,(49) is a hotly debated but often used medical intervention,(50) which can significantly improve QOL.(50-52) Utilizing substances sourced from nature i.e., minerals, and plants, homeopathic medicines have passed through a dilution process called potentization.(53) Public health regulation framing the practice and use of homeopathy in Australia is legally supported by the Therapeutic Goods Act of 1989.(54)
Until recently it was thought that homeopathic medicines were inactive dilutions beyond Avogadro's number (<10to23), but biological activity and proprieties of the initial source material are retained(55-57), hormetic activation has been observed,(57) and distinct promotion of B-cell activity has been shown,(58,59) in infection control(60) with Th1 promotion by homeopathic medicine enabling a more efficient inflammatory response, leading to resolution of disease.(61) In vitro anti-pathogenic effect of homeopathy in intestinal microbiome resistance against Escherichia coli has been observed.(62) Electron spin inversion is currently postulated as an effect measure of a homeopathic medicine within an organism.(63)
Homeopathy is used by 6.8% of Australian adults,(64) and gastrointestinal health related conditions comprise 9.3% of Australian professional homeopathic consultations, evincing alignment with health needs of the general Australian community, and highlighting IBS research as both valuable and within scope of practice.(65) Just 0.14% of the Australian research budget was spent on CM in 2012,(66) despite Australia having some of the highest rates of CM utilization in the developed world.(67) Australia's National Health & Medical Research Council 2015 homeopathy review concealed the existence of an earlier 2012 review, contained numerous instances of bias, procedural and scientific misconduct,(66) and excluded any homeopathy research experts,(68) concluding no reliable evidence for homeopathy.(69)
Homeopathy in the treatment of IBS
Two systematic reviews of homeopathy in the treatment of IBS were conducted in 2019 - Peckham et al., (70) found inconclusive evidence for efficacy or safety, and Pacheco et al., (71) noted very low certainty of evidence, but overall self-reported symptom improvement. A 2021 pilot study showed a significant decrease in severity of symptoms and pain after homeopathy treatment, highlighting the importance of individualized medicine regimens.(72) A Randomized pilot trial comparing non-individualized to individualized homeopathy (IH) was inconclusive.(73) A Randomized Controlled Trial showed clinically relevant changes in symptom severity scores in 62.5% of patients in the homeopathic treatment arm and 25% in the usual care arm.(48) Outpatient dysbiotic gut symptom improvement,(74) Australian retrospective case studies of resolved gut symptoms(75,76) and chronic candidiasis,(77) and altered dysbiotic gut microbiota,(78) achieved with homeopathy have been documented.
Homeopathy is frequently used by anxiety sufferers(79) and shows possibility of benefit in psychiatric complaints(80) such as depression and anxiety disorders.(81,82) Alleviation of stress response with homeopathy has been shown in pigs,(35) and meta-analysis identified greater efficacy for homeopathy over fluoxetine in major depressive disorder.(83)
A fibromyalgia and homeopathy RCT showed significant improvements in pain, QOL, global health and a trend toward less depression,(51) and small, but specific, treatment effects may be seen in twenty-four medical conditions for IH(84) which was found to be non-inferior to fluoxetine in the treatment of depression. An eight-year IH observational study recorded considerably increased physical and mental QOL sores, with female gender and more severe disease presentation at baseline factors predicting better therapeutic successes.(50) An Indian IH observational study associated significant benefits for patients suffering from depressive episodes,(86) and Prousky considers IH a psychotherapeutic technique.(87)
Individualized homeopathy
Individualized homeopathy (IH) is homeopathic medicine administered according to symptoms and Level of Health,(53) enabling insight into, and estimation of, pervasiveness of pathology,(88) and prognosis for both the reactions during the treatment process, and the likelihood of successful treatment.(89) Levels of Health evaluates reaction to a homeopathic medicine as improvement, moving in the right direction, or neither,(78,89) while accurately defining and classifying adverse reactions / aggravations.(90)
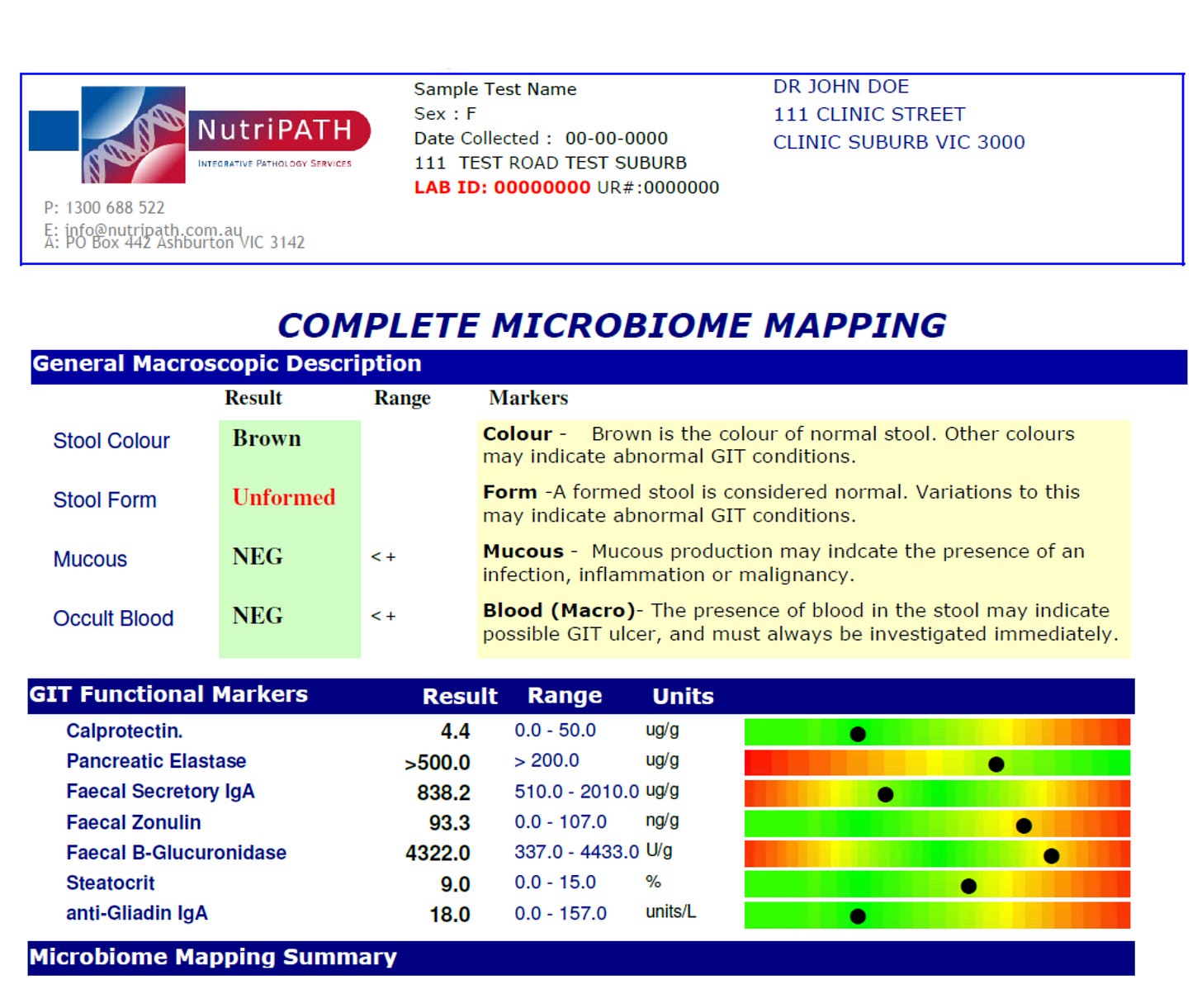
High faecal calprotectin is a very sensitive biomarker which can be used to differentiate Irritable Bowel Disease from Irritable Bowel Syndrome.(91)
Sarah Penrose BSc(hons)Hom. is an Australasian homeopath and can be contacted at goodhealthforgreatlife.com
References
1 Lacy et al., 2021. ACG Clinical Guideline: Management of Irritable Bowel Syndrome. American Journal of Gastroenterology. Jan 1;116(1):17-44. Available from https://pubmed.ncbi.nlm.nih.gov/33315591/
2 Sperber et al., 2021. Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology. Jan;160(1):99-114.e3. Available from https://pubmed.ncbi.nlm.nih.gov/32294476/
3 Canavan et al., 2014. Review article: the economic impact of the irritable bowel syndrome. Alimentary Pharmacology and Therapeutics. Nov;40(9):1023-34. Available from https://pubmed.ncbi.nlm.nih.gov/25199904/
4 Manning et al., 2020. Therapy of IBS: Is a Low FODMAP Diet the Answer? Frontiers in Psychiatry. Aug 31;11:865. Available from https://pubmed.ncbi.nlm.nih.gov/33110411/
5 Paré et al., 2006. Health-related QOL, work productivity, and health care resource utilization of subjects with irritable bowel syndrome: baseline results from LOGIC (Longitudinal Outcomes Study of Gastrointestinal Symptoms in Canada), a naturalistic study. Clinical Therapeutics. Oct;28(10):1726-35; discussion 1710-1. Available from https://pubmed.ncbi.nlm.nih.gov/17157129/
6 Sabaté et al., 2020. Expectations of IBS patients concerning disease and healthcare providers: Results of a prospective survey among members of a French patients' association. Clinics and Research in Hepatology and Gastroenterology. Nov;44(6):961-967. Available from https://pubmed.ncbi.nlm.nih.gov/32205115/
7 Mousavi et al., 2020. An update on efficacy and safety considerations for the latest drugs used to treat irritable bowel syndrome. Expert Opinion on Drug Metabolism and Toxicology. Jul;16(7):583-604. Available from https://pubmed.ncbi.nlm.nih.gov/32380874/
8 Drossman & Hasler, 2016. Rome IV-Functional GI Disorders: Disorders of Gut-Brain Interaction. Gastroenterology. May;150(6):1257-61. Available from https://pubmed.ncbi.nlm.nih.gov/27147121/
9 Mujagic et al., 2015. The Experience Sampling Method--a new digital tool for momentary symptom assessment in IBS: an exploratory study. Neurogastroenterology and Motility: the official journal of the European Gastrointestinal Motility Society. Sep;27(9):1295-302. Available from https://pubmed.ncbi.nlm.nih.gov/26100684/
10 Shulman et al., 2014. Associations among gut permeability, inflammatory markers, and symptoms in patients with irritable bowel syndrome. Journal of Clinical Gastroenterology. Nov;49(11):1467-76. Available from https://pubmed.ncbi.nlm.nih.gov/24435814/
11 Rijnaarts et al., 2021. Subtypes and Severity of Irritable Bowel Syndrome Are Not Related to Patients' Self-Reported Dietary Triggers: Results From an Online Survey in Dutch Adults. Journal of the Academy of Nutrition and Dietetics. Mar 2:S2212-2672(21)00028-9. Available from https://pubmed.ncbi.nlm.nih.gov/33674208/
12 Schwille-Kiuntke et al., 2011. Postinfectious irritable bowel syndrome: follow-up of a patient cohort of confirmed cases of bacterial infection with salmonella or Campylobacter. Neurogastroenterology and Motility. 30 August 2011. Available from https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2982.2011.01779.x
13 Thabane & Marshall., 2009. Post-infectious irritable bowel syndrome. World Journal of Gastroenterology. Aug 7;15(29):3591-6. Available from: https://pubmed.ncbi.nlm.nih.gov/19653335/
14 Ghoshal & Ghoshal., 2017. Small Intestinal Bacterial Overgrowth and Other Intestinal Disorders. Gastroenterology Clinics of North America. Mar;46(1):103-120. Available from https://pubmed.ncbi.nlm.nih.gov/28164845/
15 Botschuijver et al., 2017. Intestinal Fungal Dysbiosis Is Associated With Visceral Hypersensitivity in Patients with Irritable Bowel Syndrome & Rats. Gastroenterology. Oct;153(4):1026-1039. Available from https://pubmed.ncbi.nlm.nih.gov/28624575/
16 Sugiyama & Shiotani, 2021. The Cutting Edge Research of Functional Gastrointestinal Disorders in Japan: Review on JGA Core Symposium 2018-2020. Digestion. 102(1):6-11. Available from https://pubmed.ncbi.nlm.nih.gov/33080599/
17 Prospero et al., 2021. Somatization in patients with predominant diarrhoea irritable bowel syndrome: the role of the intestinal barrier function and integrity. BMC Gastroenterology. May 22;21(1):235. Available from https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-021-01820-7
18 Simpson et al., 2021. The gut microbiota in anxiety and depression - A systematic review. Clinical Psychology Review. Feb;83:101943. Available from https://pubmed.ncbi.nlm.nih.gov/33271426/
19 Hollister et al., 2020. Relationships of Microbiome Markers with Extraintestinal, Psychological Distress and Gastrointestinal Symptoms, and QOL in Women with Irritable Bowel Syndrome. Journal of Clinical Gastroenterology. 54(2):175-183. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6387862/
20 Liu et al., 2017. Altered molecular signature of intestinal microbiota in irritable bowel syndrome patients compared with healthy controls: A systematic review and meta-analysis. Digestive and Liver Disease. Apr;49(4):331-337. Available from https://pubmed.ncbi.nlm.nih.gov/28179092/
21 Zhuang X, Xiong L, Li L, Li M, Chen M. 2017. Alterations of gut microbiota in patients with irritable bowel syndrome: A systematic review and meta-analysis. Journal of Gastroenterology and Hepatology. Jan;32(1):28-38. Available from https://pubmed.ncbi.nlm.nih.gov/27300149/
22 Maharshak et al., 2018. Fecal and Mucosa-Associated Intestinal Microbiota in Patients with Diarrhea-Predominant Irritable Bowel Syndrome. Digestive Diseases and Science. 2018 Jul;63(7):1890-1899. Available from https://pubmed.ncbi.nlm.nih.gov/29777439/
23 Wang et al., 2019. Gut Microbial Dysbiosis in the Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis of Case-Control Studies. Journal of the Academy of Nutrition and Dietetics. Apr;120(4):565-586. Available from https://pubmed.ncbi.nlm.nih.gov/31473156/
24 Herndon et al., 2020. Targeting the gut microbiota for the treatment of irritable bowel syndrome. The Kaohsiung Journal of Medical Sciences. Mar;36(3):160-170. Available from: https://pubmed.ncbi.nlm.nih.gov/31782606/
25 Matsumoto et al., 2021. Mucosa-Associated Microbiota in Patients with Irritable Bowel Syndrome: A Comparison of Subtypes. Digestion. 102(1):49-56. Available from https://pubmed.ncbi.nlm.nih.gov/33271532/
26 Whitmont, 2020. The Human Microbiome, Conventional Medicine, and Homeopathy. Homeopathy. Nov;109(4):248-255. Available from https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0040-1709665
27 Mukhtar et al., 2019. Functional gastrointestinal disorders and gut-brain axis: What does the future hold? World Journal of Gastroenterology. Feb 7;25(5):552-566. Available from https://pubmed.ncbi.nlm.nih.gov/30774271/
28 Patel et al., 2021. Review of Treatment Options for Irritable Bowel Syndrome with Constipation and Chronic Idiopathic Constipation. International Journal of General Medicine. Apr 21;14:1457-1468. Available from https://pubmed.ncbi.nlm.nih.gov/33907450/
29 Hausteiner-Wiehle & Henningsen, 2014. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World Journal of Gastroenterology. May 28;20(20):6024-30. Available from https://pubmed.ncbi.nlm.nih.gov/24876725/
30 Simpson et al., 2020. Feeling down? A systematic review of the gut microbiota in anxiety/depression and irritable bowel syndrome. Journal of Affective Disorders. Apr 1;266:429-446. Available from https://pubmed.ncbi.nlm.nih.gov/32056910/
31 Creed et al., North of England IBS Research Group 2005. Outcome in severe irritable bowel syndrome with and without accompanying depressive, panic and neurasthenic disorders. The British Journal of Psychiatry: the journal of mental science. Jun;186:507-15. Available from https://pubmed.ncbi.nlm.nih.gov/15928362/
32 Hu et al., 2021.The level and prevalence of depression and anxiety among patients with different subtypes of irritable bowel syndrome: a network meta-analysis. BMC Gastroenterology. Jan 7;21(1):23. Available from https://pubmed.ncbi.nlm.nih.gov/33413140/
33 Vahora et al., 2020. How Serotonin Level Fluctuation Affects the Effectiveness of Treatment in Irritable Bowel Syndrome. Cureus. Aug 19;12(8):e9871. Available from https://pubmed.ncbi.nlm.nih.gov/32968548/
34 Gamble, J. 2006. Mastering Homeopathy 2; The Treatment of Irritable Bowel Syndrome. Wollongong, New South Wales. Karuna Publishing.
35 Dang & Kim., 2021. The effects of road transportation with or without homeopathic remedy supplementation on growth performance, apparent nutrient digestibility, fecal microbiota, and serum cortisol and superoxide dismutase levels in growing pigs. Journal of Animal Science. Apr 1;99(4):skab077. Available from https://academic.oup.com/jas/article-abstract/99/4/skab077/6162474?redirectedFrom=fulltext
36 Lovell & Ford, 2012. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clinical Gastroenterology and Hepatology: the official clinical practice journal of the American Gastroenterological Association. Jul;10(7):712-721.e4. Available from https://www.cghjournal.org/article/S1542-3565(12)00308-4/fulltext
37 Boyce et al., 2006. Epidemiology of the functional gastrointestinal disorders diagnosed according to Rome II criteria: an Australian population-based study. Internal Medicine Journal. Jan;36(1):28-36. Available from https://pubmed.ncbi.nlm.nih.gov/16409310/
38 Oka et al., 2020. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. The Lancet. Gastroenterology and Hepatology. Oct;5(10):908-917. Available from https://pubmed.ncbi.nlm.nih.gov/32702295/
39 Scaciota et al., 2021. Interventions for the treatment of irritable bowel syndrome: A review of Cochrane systematic reviews. Arquivos de Gastroenteroliga. Jan-Mar;58(1):120-126. Available from https://www.scielo.br/j/ag/a/Ky4jb7vB5ntYRfZYZgJxX5d/?lang=en
40 Thomas & Luthin, 2015. Current and emerging treatments for irritable bowel syndrome with constipation and chronic idiopathic constipation: focus on prosecretory agents. Pharmacotherapy. Jun;35(6):613-30. Available from: https://pubmed.ncbi.nlm.nih.gov/26016701/
41 Fairbrass et al., 2020. Prevalence of irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease in remission: a systematic review and meta-analysis. The Lancet. Gastroenterology and Hepatology. Dec;5(12):1053-1062. Available from https://pubmed.ncbi.nlm.nih.gov/33010814/
42 Black et al., 2020. Efficacy of psychological therapies for irritable bowel syndrome: systematic review and network meta-analysis. Gut. Aug;69(8):1441-1451. Available from https://pubmed.ncbi.nlm.nih.gov/32276950/
43 Peters et al., 2016. Randomised clinical trial: the efficacy of gut-directed hypnotherapy is similar to that of the low FODMAP diet for the treatment of irritable bowel syndrome. Alimentary Pharmacology and Therapeutics. Sep;44(5):447-59. Available from https://pubmed.ncbi.nlm.nih.gov/27397586/
44 Billings et al., 2020. Potential Benefit With Complementary and Alternative Medicine in Irritable Bowel Syndrome: A Systematic Review and Meta-analysis. Clinical Gastroenterology and Hepatology: the official clinical practice journal of the American Gastroenterological Association. Sep 19:S1542-3565(20)31296-9. Available from https://pubmed.ncbi.nlm.nih.gov/32961342/
45 Alonso-Cotoner et al., 2021. The Role of Purported Mucoprotectants in Dealing with Irritable Bowel Syndrome, Functional Diarrhea, and Other Chronic Diarrheal Disorders in Adults. Advances in Therapy. May;38(5):2054-2076. Available from https://pubmed.ncbi.nlm.nih.gov/33738725/
46 Bu et al., 2020. A critical review on the relationship of herbal medicine, Akkermansia muciniphila, and human health. Biomedicine and Pharmacotherapy. Aug;128:110352. Available from https://www.sciencedirect.com/science/article/pii/S075333222030545X?via%3Dihub
47 Pei et al., 2020. Effect of Acupuncture in Patients with Irritable Bowel Syndrome: A Randomized Controlled Trial. Mayo Clinic Proceedings. Aug;95(8):1671-1683. Available from https://pubmed.ncbi.nlm.nih.gov/32499125/
48 Peckham et al., 2014. Interim results of a randomised controlled trial of homeopathic treatment for irritable bowel syndrome. Homeopathy. Jul;103(3):172-7. Available from https://pubmed.ncbi.nlm.nih.gov/24931748/
49 NCCIH. 2021. Homeopathy: what you need to know. National Centre for Complementary and Integrative Health. U.S Department of Health and Human Services. Maryland. Available from: https://www.nccih.nih.gov/health/homeopathy
50 Witt et al., 2008. How healthy are chronically ill patients after eight years of homeopathic treatment?--Results from a long term observational study. BMC Public Health. Dec 17;8:413. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2630323/
51 Bell et al., 2004. Improved clinical status in fibromyalgia patients treated with individualized homeopathic remedies versus placebo. Rheumatology (Oxford). May;43(5):577-82. Available from https://academic.oup.com/rheumatology/article/43/5/577/1788410
52 Frass et al., 2020. Homeopathic Treatment as an Add-On Therapy May Improve QOL and Prolong Survival in Patients with Non-Small Cell Lung Cancer: A Prospective, Randomized, Placebo-Controlled, Double-Blind, Three-Arm, Multicenter Study. Oncologist. Dec;25(12):e1930-e1955. Available from https://pubmed.ncbi.nlm.nih.gov/33010094/
53 Văcăraș et al., 2020. Myasthenia gravis therapy with individualized homeopathy: A case report. Clinical Case Reports. Jul 29;8(12):2464-2468. Available from https://onlinelibrary.wiley.com/doi/10.1002/ccr3.3190
54 Australian Government Department of Health. Federal Register of Legislation. 2021. Therapeutic Goods Act 1989; No. 21 1990 as amended Commonwealth of Australia. Canberra. Available from https://www.legislation.gov.au/Details/C2014C00102
55 Chikramane et al., 2010. Extreme homeopathic dilutions retain starting materials: A nanoparticulate perspective. Homeopathy. Oct;99(4):231-42. Available from https://www.thiemeconnect.com/products/ejournals/abstract/10.1016/j.homp.2010.05.006
56 Tournier & Roberts, 2015. Chemical dyes can detect presence of homeopathic high dilutions. Homeopathy Research Institute. 30; 1-2. Available from: https://www.hri-research.org/wpcontent/uploads/2015/12/HRI_ResearchArticle_30_TournierRoberts_2015_SolvatochromicDyes1.pdf
57 Kalliantas et al., 2021. Micro-nano particulate compositions of Hypericum perforatum L in ultra high diluted succussed solution medicinal products. Heliyon. Apr 19;7(4):e06604. Available from https://www.sciencedirect.com/science/article/pii/S2405844021007076
58 Rodrigues de Santana et al., 2014. Modulation of inflammation response to murine cutaneous Leishmaniasis by homeopathic medicines: Antimonium crudum 30cH. Homeopathy. Oct;103(4):264-74. Available from https://pubmed.ncbi.nlm.nih.gov/25439043/
59 de Santana et al., 2017. High dilutions of antimony modulate cytokines production and macrophage - Leishmania (L.) amazonensis interaction in vitro. Cytokine. Apr;92:33-47. Available from https://pubmed.ncbi.nlm.nih.gov/28092793/
60 Cajueiro et al., 2017. Homeopathic medicines cause Th1 predominance and induce spleen and megakaryocytes changes in BALB/c mice infected with Leishmania infantum. Cytokine. Jul;95:97-101. Available from https://pubmed.ncbi.nlm.nih.gov/28254560/
61 Mahesh S, Mahesh M, Vithoulkas G. 2018 (b). Could Homeopathy Become An Alternative Therapy In Dengue Fever? An example Of 10 Case Studies. Journal of Medicine and Life. Jan-Mar;11(1):75-82. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5909950/
62 Buchheim-Schmidt et al., 2021. In vitro evaluation of the anti-pathogenic activity of Okoubaka aubrevillei on the human gastrointestinal tract. Zeitschrift fur Gastroenterologie. May;59(5):423-437. English. Available from https://www.thieme-connect.com/products/ejournals/abstract/10.1055/a-1404-3344
63 Vithoulkas & Berghian-Grosan, 2020. The Spin of Electrons and the Proof for the Action of Homeopathic Remedies. Journal of Medicine and Life. Jul-Sep;13(3):278-282 Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7550134/
64 Steel et al., 2018. Complementary medicine use in the Australian population: Results of a nationally-representative cross-sectional survey. Scientific reports. 8(1), 17325. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6251890/
65 Salter et al., 2020. Sustaining Homeopathy in Australia: Results and Analysis of First National Practice Survey. Similia, The Australian Journal of Homeopathic Medicine. 32,1;23-29. Hobart. The Australian Homeopathic Association.
66 Australian Homeopathic Association. 2017. The National Health & Medical Research Council (NHMRC) and Research Integrity. Hobart. Available from http://www.nhmrchomeopathy.com/
67 Andrews et al., 2012. The Profile of Complementary and Alternative Medicine Users and Reasons for Complementary and Alternative Medicine Use. In: Adams J, Andrews G, Barnes J, Magin P, Broom A, editors. Traditional, Complementary and Integrative Medicine: An International Reader. London: Palgrave Macmillan. Available from https://books.google.com.au/books hl=en&lr=&id=PyYdBQAAQBAJ&oi=fnd&pg=PP1&ots=GFkANwfHjc&sig=YJzT6ZdZQc6Doa1tpWFWIBqai4g&redir_esc=y#v=onepage&q&f=false
68 Homeopathy Research Institute. 2021. The Australian Report. Homeopathy Research Institute. Kensington, London. Available from https://www.hriresearch.org/resources/homeopathy-the-debate/the-australian-report-on-homeopathy/
69 NHMRC. 2021. Homeopathy. National Health and Medical Research Council. Australian Government Canberra. Available from https://www.nhmrc.gov.au/about-us/resources/homeopathy
70 Peckham et al., 2019. Homeopathy for treatment of irritable bowel syndrome. Cochrane Database Systematic Reviews. Sep 4;9(9):CD009710. Available from https://pubmed.ncbi.nlm.nih.gov/31483486/
71 Pacheco et al., 2019. What do Cochrane systematic reviews say about the management of irritable bowel syndrome? Sao Paulo Medical Journal. May 8;137(1):82-91. Available from https://www.scielo.br/j/spmj/a/CKGfwTGgHcbvRtSn49qMRvx/?lang=en
72 Martínez-Islas et al., 2021. Evaluation of Individualized Homeopathic Treatment in Patients With Irritable Bowel Syndrome: A Pilot Study. Altern Ther Health Med. Jun;27(S1):158-161. Available from: https://pubmed.ncbi.nlm.nih.gov/33711816/
73 Nahar et al., 2019. An open-label randomized pragmatic non-inferiority pilot trial to compare the effectiveness of Dysentery compound with individualized homeopathic medicines in irritable bowel syndrome. Journal of Complementary and Integrative Medicine. Jun 14;16(4):/j/jcim.2019.16.issue-4/jcim-2018-0217/jcim-2018-0217.xml. Available from https://www.degruyter.com/document/doi/10.1515/jcim-2018-0217/html
74 Uchiyama-Tanaka, 2018. Case Study of Homeopathic Bowel Nosode Remedies for Dysbiotic Japanese Patients. Journal of Alternative and Complementary Medicine. Feb;24(2):187-192. Available from https://www.liebertpub.com/doi/10.1089/acm.2017.0061?url_ver=Z39.882003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
75 Gamble, J. 2019. The Gut: Cases and Clinical Experience. A reflection on Gut Disease over Three Decades. Similia, The Australian Journal of Homeopathic Medicine. 31, 1; 5 - 11. Hobart. The Australian Homeopathic Association.
76 Penrose, S. 2019. Drugs, Dysbiosis and the Bowel Nosodes. The Australian Journal of Homeopathic Medicine, 31 (1), 12-18. Hobart. The Australian Homeopathic Association.
77 Levy, D. 2019. Chronic candidiasis and Ulcerative Colitis – Two cases. The Australian Journal of Homeopathic Medicine, 31 (1), 26-28. Hobart. The Australian Homeopathic Association.
78 Penrose, S. 2021. Insomnia, Candida Parapsilosis and other Nosocomial Infections – A Levels of Health Case Analysis. Similia, The Australian Journal of Homeopathic Medicine. 34, 1; 41 - 46. Hobart. The Australian Homeopathic Association.
79 Pilkington et al., 2006. Homeopathy for anxiety and anxiety disorders: a systematic review of the research. Homeopathy. Jul;95(3):151-62. Available from https://pubmed.ncbi.nlm.nih.gov/27397586/
80 Davidson et al., 2011. Homeopathic treatments in psychiatry: a systematic review of randomized placebo-controlled studies. Journal of Clinical Psychiatry. Jun;72(6):795-805. Available from https://pubmed.ncbi.nlm.nih.gov/21733480/
81 Hock & Juckel, 2018. Homöopathie bei psychiatrischen Patienten – Für und Wider [Homeopathy for psychiatric patients-for and against]. Der Nervenarzt. Sep;89(9):1014-1019. Available from https://pubmed.ncbi.nlm.nih.gov/29858643/
82 Parewa et al., 2021. Individualized Homeopathic Medicines in the Treatment of Generalized Anxiety Disorder: A Double-Blind, Randomized, Placebo-Controlled, Pilot Trial. Complementary Medicine Research. Mar 4:1-11. Available from https://pubmed.ncbi.nlm.nih.gov/33662951/
83 Rotella et al., 2020. Homeopathic Remedies in Psychiatric Disorders: A Meta-analysis of Randomized Controlled Trials. Journal of Clinical Psychopharmacology. May/Jun;40(3):269-275. Available from: https://pubmed.ncbi.nlm.nih.gov/32332462/
84 Mathie et al. 2014. Randomised placebo-controlled trials of individualised homeopathic treatment: systematic review and meta-analysis. Systematic Reviews. 3, 142. Available from: https://pubmed.ncbi.nlm.nih.gov/25480654/
85 Mathie et al. 2017. Randomised, double-blind, placebo-controlled trials of non-individualised homeopathic treatment: systematic review and meta-analysis. Systematic Reviews. 6 (1), 63. Available from: https://pubmed.ncbi.nlm.nih.gov/28340607/
86 Oberai et al. 2013. Homoeopathic management in depressive episodes: A prospective, unicentric, non-comparative, open-label observational study. Indian Journal of Research in Homeopathy. 7:116-125. Available from https://www.ijrh.org/article.asp?issn=09747168;year=2013;volume=7;issue=3;spage=116;epage=125;aulast=Oberai
87 Prousky, 2018. Repositioning Individualized Homeopathy as a Psychotherapeutic Technique With Resolvable Ethical Dilemmas. Journal of Evidence Based Integrative Medicine. Dec;23:2515690X18794379. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6111390/
88 Chabanov et al., 2018. Levels of Health Theory With the Example of a Case of Juvenile Rheumatoid Arthritis. Journal of Evidence Based Integrative Medicine. Jan-Dec;23:2515690X18777995. Available from https://journals.sagepub.com/doi/10.1177/2515690X18777995?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
89 Vithoulkas, 2017. Levels of Health, The second volume of the Science of Homeopathy, revised edition. Alonissos: International Academy of Classical Homeopathy.
90 Teut et al., 2020. Recommendations for Designing, Conducting and Reporting Observational Studies in Homeopathy. Homeopathy. Aug;109(3):114-125. Available from https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0040-1708045
91 Pathirana et al., 2018. Faecal Calprotectin. The Clinical biochemist. Reviews. 39(3),77-90.Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6370282/