Faecal microbiotal community composition is variable,(1) uniquely individual,(2) and links to stool consistency, extra-intestinal symptoms and Quality of Life (QOL) in women with Irritable Bowel Syndrome (IBS).(3) Microbiome change in IBS patients may determine patterns of brain activation,(4) with higher diversity equating to better QOL.(3)
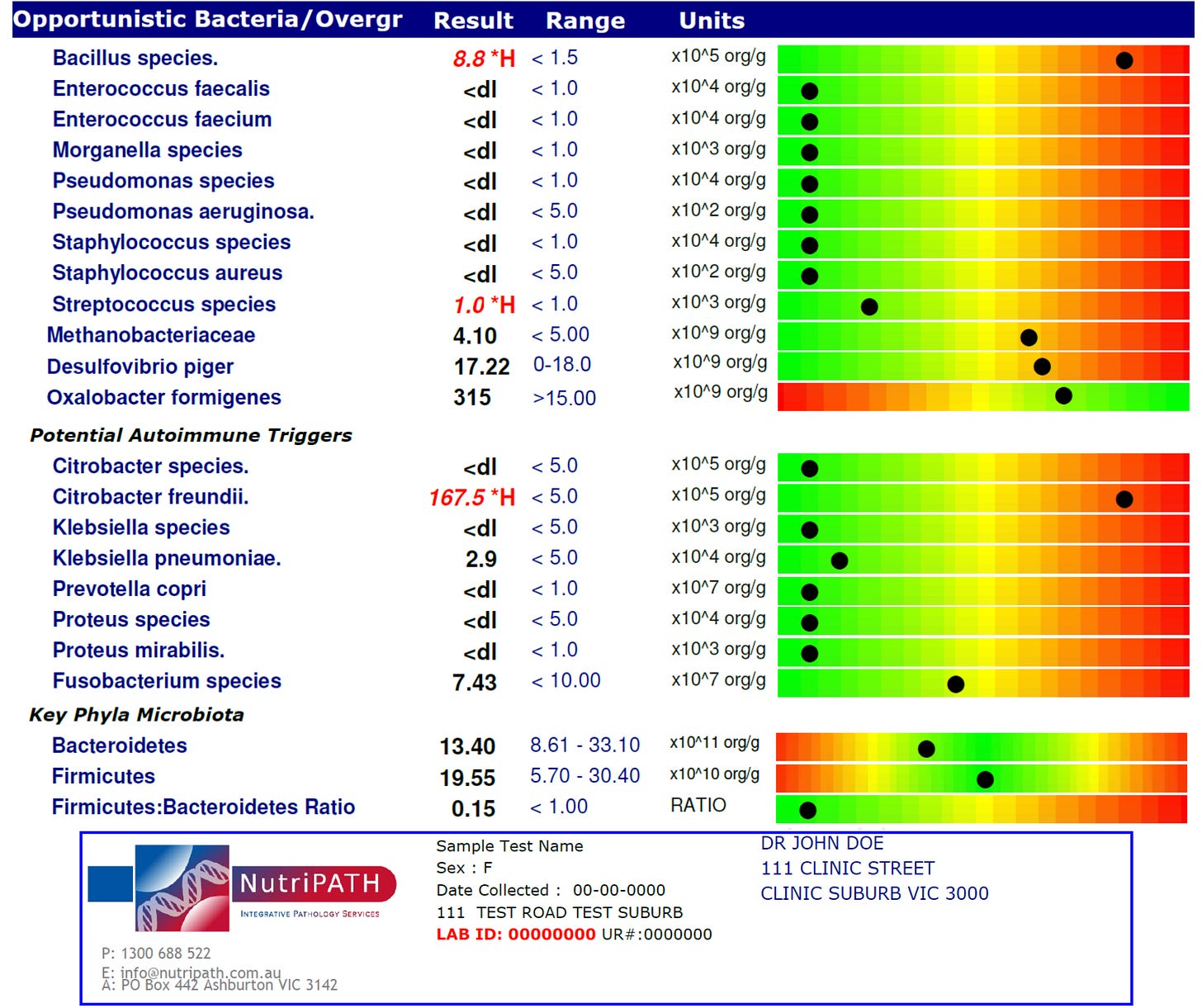
There is an absence of a gold standard in faecal microbiota profiling protocols.(5) NutriPATH laboratory offers a range of testing including Complete Microbiome Mapping - consisting of DNA quantitative polymerase chain reaction (q-PCR), enzyme-linked immunosorbent assay (ELISA), and Gas chromatography-mass spectrometry (GC-MS).(6)
Firmicutes and Bacteroidetes represent 90% of gastrointestinal microbiota phyla.(2) Firmicutes: Bacteroidetes (FB) ratios, associated with dysbiosis(7) are found to be significantly decreased in gastrointestinal disorders(8) and characteristic of IBS,(9-15) however, FB ratios can remain similar while abundance of both taxa is increased or decreased therefore alpha diversity - the most bacterial taxa within a single sample(16) can be used to detect abundance of individual faecal microbiotal communities.(17)
According to Dr. Russel Malcom ‘the dysbiotic case is a blocked case. Patient’s whose intestinal ecosystem is significantly disordered have an on-board source of immunological and physiological chaos. If the symbiotic homeostasis is not corrected, the patient will be incapable of responding to a classical simillimum. Or the response will be weak and short-lived.’(18)
Vithoulkas’ Levels of Health theory places people susceptible to infection by staphylococcus in Group A, however, if its treatment compromises the immune system, descent through the Levels of Health begins. The very first introduction of chemical drugs to an organism impedes the free will of its defences, forcing it to rearrange and muster the next best line of resistance to keep the disturbance away from vital organs. If peripheral expression is obfuscated the organism is forced to concede and will manifest symptoms on a deeper level.(19)

Group B is highly susceptible to fungal infections such as candida spp., and develops prolific infestations, with microorganisms becoming more and more virulent and resistant to antibiotics. Group D is often subject to nosocomial bacterial or viral infection which have modified and become resistant.(19)
Enterococcus spp. are inherently resistant to a number of antimicrobials with a few isolates having multi-drug resistance.(20) Enterococcus faecalis is the most common nosocomial infection after Escherichia coli(21) - the theme of over exposure to hospital environments leads right to the bowel nosode Faecalis (Bacillus Faecalis Alcilagenes), which has the concomitant theme of inherited dysbiosis.(18)
Candida parapsilosis is a nosocomial infection renowned for its capacity to form biofilms on catheters and medical devices or fluids, with the hands of health care workers also major vectors of transmission. Low-birth-weight neonates are at greatest risk of C. parapsilosis infection which is implicated as causing over one-quarter of all invasive fungal infections in low-birth-weight infants in the UK.(22)
In Australia, C. parapsilosis is involved in 16.5% of all Candida spp. bloodstream infections with heavy fungal burdens typically lacking severe inflammation, and may also be present in the blood, intestines and lungs.(23) SENTRY data showed just 0.6% of C. parapsilosis isolates from the Asia Pacific region have resistance to fluconazole and therefore is not classed as a resistant infection.(24) The clinical picture of C. parapsilosis infection includes respiratory dysfunction and apnoea, with the homeopathic remedy showing symptoms of: Extreme agitation; explosive anger; and irritability.(25)
Jon Gamble writes that a person with pre-existing gut dysbiosis is pre-disposed to intestinal parasites because disturbances in gut flora undermine its functional immunity, creating an ideal environment for parasitic infection, and, unless the susceptibility of the person changes, symptoms will eventually return as they find the host a very welcoming home.(26)
Sarah’s papers ‘Insomnia, Candida Parapsilosis and other Nosocomial Infections – A Levels of Health Case Analysis’(27) and ‘Drugs, Dysbiosis and the Bowel Nosodes’ examining nine cases of resolved gut disturbance(28) have been published in Similia, The Australian Journal of Homeopathic Medicine.
Complete Microbiome Mapping in Australia is by NUTRIPATH.com.au, and via NUTRISEARCH.co.nz in New Zealand.
Sarah Penrose BSc(hons)Hom. is an Australasian homeopath and can be contacted at goodhealthforgreatlife.com
References
1 Rinninella et al., 2019. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms. Jan 10;7(1):14 Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6351938/
2 Arumugam et al., 2011. Enterotypes of the human gut microbiome. Nature. May 12;473(7346):174-80. Available from https://pubmed.ncbi.nlm.nih.gov/21508958/
3 Hollister et al. 2020. Relationships of Microbiome Markers with Extraintestinal, Psychological Distress and Gastrointestinal Symptoms, and QOL in Women with Irritable Bowel Syndrome. Journal of Clinical Gastroenterology. 54(2):175-183. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6387862/
4 Labus et al., 2017. Differences in gut microbial composition correlate with regional brain volumes in irritable bowel syndrome. Microbiome. May 1;5(1):49. Available from https://pubmed.ncbi.nlm.nih.gov/28457228/
5 Mancabelli et al., 2017. Identification of universal gut microbial biomarkers of common human intestinal diseases by meta-analysis. FEMS Microbiology Ecology. Dec 1;93(12). Available from https://pubmed.ncbi.nlm.nih.gov/29126267/
6 NutriPATH, Integrative and functional pathology services. 2020b. (Test code 2206) Complete microbiome mapping Test Method. Burwood; Victoria. Available from: https://www.nutripath.com.au/product/complete-microbiome-mapping/
7 Stojanov et al., 2020. The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease. Microorganisms. 8(11), 1715. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7692443/
8 Laswi et al., 2021. A Comparative Pilot Study of Bacterial and Fungal Dysbiosis in Neurodevelopmental Disorders and Gastrointestinal Disorders: Commonalities, Specificities and Correlations with Lifestyle. Microorganisms. Apr 2;9(4):741. Available from https://pubmed.ncbi.nlm.nih.gov/33918112/
9 Maukonen et al., 2006. Prevalence and temporal stability of selected clostridial groups in irritable bowel syndrome in relation to predominant faecal bacteria. Journal of Medical Microbiology. May;55(Pt 5):625-633. Available from https://pubmed.ncbi.nlm.nih.gov/33271532/
10 Rajilić-Stojanović et al., 2011. Global and deep molecular analysis of microbiota signatures in fecal samples from patients with irritable bowel syndrome. Gastroenterology. Nov;141(5):1792-801. Available from https://pubmed.ncbi.nlm.nih.gov/21820992/
11 Jeffery et al., 2012. An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut. Jul;61(7):997-1006. Available from https://pubmed.ncbi.nlm.nih.gov/22180058/
12 Lee & Lee, 2014. Intestinal microbiota in pathophysiology and management of irritable bowel syndrome. World Journal of Gastroenterology. Oct Jul 21;20(27):8886-97. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4112865/
13 Pozuelo et al., 2015. Reduction of butyrate- and methane-producing microorganisms in patients with Irritable Bowel Syndrome. Scientific Reports. Aug 4;5:12693. Available from https://pubmed.ncbi.nlm.nih.gov/26239401/
14 Liu et al., 2017. Altered molecular signature of intestinal microbiota in irritable bowel syndrome patients compared with healthy controls: A systematic review and meta-analysis. Digestive and Liver Disease. Apr;49(4):331-337. Available from https://pubmed.ncbi.nlm.nih.gov/28179092/
15 Duan et al., 2019. Alterations of Gut Microbiota in Patients With Irritable Bowel Syndrome Based on 16S rRNA-Targeted Sequencing: A Systematic Review. Clinical and Translational Gastroenterology. Feb;10(2):e00012. Available from https://pubmed.ncbi.nlm.nih.gov/30829919/
16 Walters & Martiny, 2020. Alpha-, beta-, and gamma-diversity of bacteria varies across habitats. PLoS One. Sep 23;15(9):e0233872. Available from https://pubmed.ncbi.nlm.nih.gov/24646513/
17 Zheng et al., 2021. Characterization on gut microbiome of PCOS rats and its further design by shifts in high-fat diet and dihydrotestosterone induction in PCOS rats. Bioprocess and Biosystems Engineering. May;44(5):953-964. Available from https://link-springer-com.rsm.idm.oclc.org/article/10.1007/s00449-020-02320-w
18 Malcom R. Systems & Symbiosis - The Bowel Nosodes Reappraised. A Seminar in Integrative Medicine. Centre for Integrative Medical Training ltd. RLHH Education. 2002. Available from https://www.rlhh-education.com/backend/web/images/product-materials/core2007_20171109171404491.pdf
19 Vithoulkas, G. 2017. Levels of Health, The second volume of the Science of Homeopathy, revised edition. Alonissos: International Academy of Classical Homeopathy.
20 Zaheer et al. 2020. Surveillance of Enterococcus spp. reveals distinct species and antimicrobial resistance diversity across a One-Health continuum. Nature, Scientific Reports. 2019. https://www.nature.com/articles/s41598-020-61002-5#citeas
21 Vermeulen, F. Monera, Kingdom Bacteria & Viruses, Spectrum Materia Medica; Volume 1. Haarlem: Emryss Publishers; 2005.
22 Trofa et al. Candida parapsilosis, an emerging fungal pathogen. Clinical microbiology reviews. 2008. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2570155/
23 Tóth et al. Candida parapsilosis: from Genes to the Bedside. Clinical microbiology reviews 2019. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6431126/
24 Michael et al. Twenty Years of the SENTRY Antifungal Surveillance Program: Results for Candida Species from 1997–2016, Open Forum Infectious Diseases. 2019. https://academic.oup.com/ofid/article/6/Supplement_1/S79/5381621
25 Vermeulen, F. Fungi, Kingdom Fungi, Spectrum Materia Medica; Volume 2. Haarlem: Emryss Publishers; 2007.
26 Gamble, J. Mastering Homeopathy 2; The Treatment of Irritable Bowel Syndrome. Wollongong; Karuna publishing; 2006.
27 Penrose, S. 2021. Insomnia, Candida Parapsilosis and other Nosocomial Infections – A Levels of Health Case Analysis. Similia, The Australian Journal of Homeopathic Medicine. 34, 1; 41 - 46. Hobart. The Australian Homeopathic Association.
28 Penrose, S. 2019. Drugs, Dysbiosis and the Bowel Nosodes. Similia, The Australian Journal of Homeopathic Medicine, 31 (1), 12-18. Hobart. The Australian Homeopathic Association.